IIAV.nl
Vergelijk onafhankelijk +15.000 producten
IIAV.nl is de plek voor het vinden van de scherpste deal tegen de beste levervoorwaarden. Vergelijk producten van betrouwbare retailers in Nederland & profiteer direct van kortingen die oplopen tot in de honderden euro’s!
- Vergelijk onafhankelijk +15.000 producten bij de grootste retailers
- Actuele informatiegidsen met product reviews
- Pak de scherpste deal tegen de beste levervoorwaarden
Ruim & kwaliteit aanbod
Vergelijk 10.000+ producten
Gratis prijzen vergelijken
Vergelijk de grootste retailers in NL
Pak de scherpste deal
Nooit meer teveel betalen
Beste levervoorwaarden
Ga voor de beste levervoorwaarden
Populaire categorieën
Actuele aankoopgidsen

De Voor- en Nadelen van Pre Workout Supplementen
Pre workout supplementen zijn erg populair onder sporters, vooral diegenen die zich bezighouden met intensieve trainingen en krachtsport. Deze supplementen zijn ontworpen om de prestaties

Wat zijn je rechten als consument bij de aanschaf van retailproducten?
Als je iets koopt in een winkel of online, heb je als consument bepaalde rechten. Een van deze rechten is het recht op garantie. Garantie

Gepersonaliseerde sieraden: unieke cadeau-ideeën voor bijzondere gelegenheden
Sieraden hebben altijd al een speciale betekenis gehad als cadeau voor geliefden bij belangrijke mijlpalen in het leven, denk bijvoorbeeld maar eens aan speciale moeder dochter

iPhone 14: Voor wie is het de ideale upgrade?
Je hebt vast en zeker al iets gezien of gehoord over de introductie van de iPhone 14. En dat is ook helemaal niet zo gek als

Wat is een goede manier om dieven buiten de deur te houden?
Wist jij dat het aantal woninginbraken in Nederland nog altijd heel hoog ligt? Ieder jaar worden mensen het slachtoffer van mensen die hun woning binnendringen

Hoe kun je Apple AirPods verbinden
Als mijn Apple Airpods ooit verbindingsproblemen ondervinden, weet ik precies hoe ik ze moet oplossen. Het enige wat ik moet doen is de Bluetooth-koppeling handmatig

Hoe sluit je een monitor aan op je Mac?
Als u uw beeldschermmogelijkheden voor uw Apple MacBook of iMac wilt uitbreiden, hoeft u niet verder te zoeken. Een nieuwe monitor aansluiten hoeft niet moeilijk te

Hoe kun je bedrade oordopjes het beste gebruiken?
Wanneer je je bedrade oordopjes gebruikt, is er geen houden aan het hoogwaardige geluid dat er doorheen komt. Geniet ten volle van uw favoriete muziek

Waar let je op bij het kiezen van het schermformaat van je monitor?
Bij de keuze van de perfecte monitor voor uw werkplek is de grootte van het scherm van het grootste belang. Dit kan van grote invloed

Hoe kun je een magnetron het beste schoonmaken?
Het schoonmaken van uw magnetron hoeft geen moeizaam karwei te zijn! Met de volgende tips kan het verrassend eenvoudig en snel. Het is essentieel om

3 tips die je helpen wanneer je laptop vastloopt
Loopt uw laptop regelmatig vast? Dan wilt u daar zeker snel iets aan doen. Gelukkig kan dit probleem in veel gevallen eenvoudig worden verholpen met

Wat zijn de afmetingen van een magnetron?
Bij het kopen van een magnetron is het belangrijk rekening te houden met de afmetingen. Ingebouwde magnetrons moeten perfect in de kast passen; dit kan

3 tips om de opslagcapaciteit van je laptop te vergroten
Wanneer uw laptop de grens van de beschikbare opslagruimte bereikt, hoeft u niet in paniek te raken. Met tal van alternatieven om de hoeveelheid geheugenruimte

De verschillen tussen een over ear en on ear koptelefoon
Bij het kiezen van de perfecte hoofdtelefoon heb je twee opties: on-ear en over-ear. Hoewel oortelefoons lichter zijn dan hun tegenhangers, bieden ze minder geluidsisolatie.

Hoe kun je een koelkast inbouwen?
Een koelkast inbouwen in een bestaande keuken kan zonder gedoe. Hieronder hebben we stap-voor-stap instructies geschetst voor het zelf installeren van een inbouwkoelkast! Maar als

Bent u op zoek naar draagbaar geluid, maar weet u niet zeker hoe u de beste optie moet kiezen? Zoek niet verder! Wij hebben mobiele

Koptelefoon

Router

Tablet

Wasmachine

Digitale camera

Vriezer

Laptop

Smartwatch

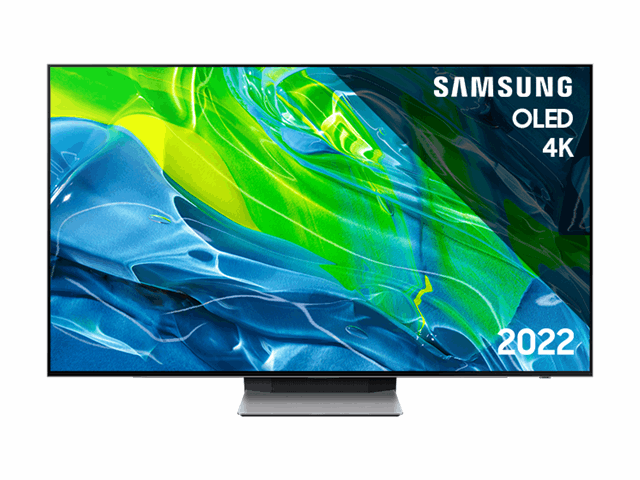
TV

Stofzuiger

Fornuis

Wasdroger

Monitor

Soundbar

Espressomachines

Actioncam

Keukenmachine

Mobiele airco

Oordopjes

Speaker

Koelkast

Afzuigkap

Vaatwasser

Magnetron
Andere bekeken zojuist
Ben je op zoek naar uniekere aanbiedingen met betrekking tot online spellen, een online casino iDeal of consoles? We raden je aan om gebruik te maken van onze zoekfunctie & te profiteren van onze meest recente updates in de categorie beeld & geluid.
Best beoordeeld

v.a. €245,- Win bij nieuwe-casinos.net
Waarom vergelijken bij IIAV.nl?
Iedereen verdient het om een eerlijke prijs te betalen voor de producten die hij/zij wil kopen. Wij maken het voor iedereen toegankelijk om eenvoudig en snel meer dan 10.000 producten te vergelijken zoals een elektrische step of vloeren van Vloerenbaas bij diverse aanbieders, zodat je nooit meer te veel betaald.
Wij houden het aanbod en de prijzen van alle elektronica producten altijd up-to-date, zodat je ook de nieuwste modellen direct mee kunt nemen in de vergelijking.
Voor vragen, opmerkingen of aanmerking kun je altijd contact opnemen met onze helpdesk. Zodoende houden wij onze service op het hoogste niveau.
Met 128-bit SSL beveiliging met geavanceerde encryptie ben je zeker van een veilige aankoop. Kies uit één van de velen betaalmogelijkheden.
Populairste producten
A-merken assortiment
Bij IIAV.nl vergelijk je alleen de beste merken van dit moment. De kwaliteit van de producten zoals een geweldige laptop of nieuwe SUP boards die je bij ons kunt vergelijken wordt hierdoor gewaarborgd!